Protein C Test

Synonyms
PC, Protein C Antigen, Protein C, Functional, Protein C Test
Applies To
Protein Ca, Tissue Plasminogen Activator (t-PA)
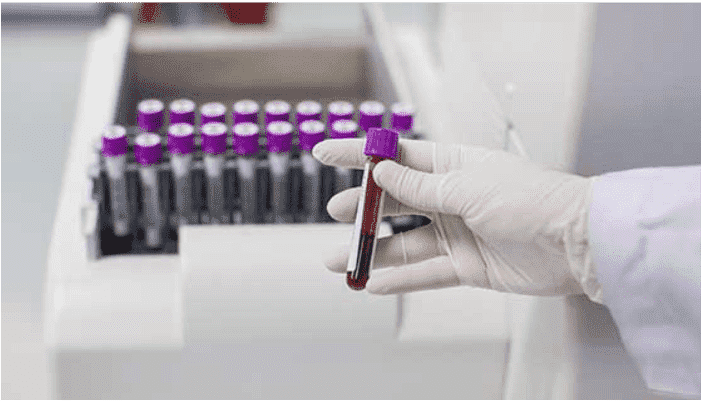
Specimen
Plasma
Container
Blue top (sodium citrate) tube
Collection
Venipuncture. Coagulation studies should be collected last if multiple tests are being drawn.
For coagulation-only tests, use a double-syringe/tube technique: draw 1–2 mL into a Vacutainer® tube and discard before collecting the test sample. This avoids tissue thromboplastin contamination.
Storage Instructions
Stable at -70°C for up to 1 month.
Reason to Reject Sample
Heparin therapy (except in chromogenic substrate-based techniques).
Turnaround Time
Approximately 1 hour
Special Instructions
Check for oral anticoagulant use. Vitamin K-dependent Protein C levels may decrease due to coumarin-based anticoagulants.
Heparin does not significantly affect snake venom-activated chromogenic methods.
Reference Range
- Adults: 0.60 – 1.13 units/mL
- 1–5 years: 0.40 – 0.92 units/mL
- 6–10 years: 0.45 – 0.93 units/mL
- 11–16 years: 0.55 – 1.11 units/mL
Use
To evaluate patients with venous thrombosis or suspected hypercoagulable conditions, especially in younger adults.
Limitations
Protein C levels may be lowered by Coumadin. Interpretation should consider anticoagulant use.
Methodology
- Enzyme-linked immunosorbent assay (ELISA)
- Radioimmunoassay (RIA)
- Rocket immunoelectrophoresis (Laurell)
- Particle concentration fluorescent immunoassay
Additional Information
Protein C is a vitamin K-dependent zymogen with anticoagulant and profibrinolytic properties. Once activated (Protein Ca), it inactivates factors Va and VIIIa, limiting thrombin formation and promoting t-PA activity for fibrinolysis.
It is synthesized in the liver and activated on the endothelium via thrombomodulin-thrombin complex. Protein Ca works synergistically with Protein S.
Deficiency Types:
– Homozygous deficiency (e.g., purpura fulminans in neonates)
– Type I (quantitative deficiency)
– Type II (normal antigen, reduced function)
Associated Conditions:
– Coumadin-induced skin necrosis
– Liver disease
– Nephrotic syndrome
– Sickle cell crises (transient consumption)
– Diabetic vs membranous glomerulopathy (protein C/S changes differ)
References
- Berdeaux DH, et al. Am J Clin Pathol, 1993; 99:677–86.
- Brenner B, et al. Am J Obstet Gynecol, 1987; 157:1160–1.
- Civantos F, et al. ASCP Check Sample, 1987.
- Clouse LH & Comp PC. N Engl J Med, 1986; 314:1298–1300.
- Esmon NL. Prog Hemost Thromb, 1989; 9:29–55.
- Harrison RL & Alperin JB. Am J Hematol, 1992; 40(1):33–7.
- Hill RT & Ens GE. Clin Hemost Rev, 1987; 1:1–6.
- Manco-Johnson M, et al. Am J Hematol, 1992; 40(1):69–70.
- Marchetti G, et al. Br J Haematol, 1993; 84:285–9.
- Melissari E & Kakkar VV. Br J Haematol, 1989; 72(2):222–8.
- Rosenberg RD & Bauer KA. Hosp Pract, 1986; 21:131–47.
- Schofield KP, et al. Clin Lab Haematol, 1987; 9:255–62.
- Tollefson DFJ, et al. Arch Surg, 1988; 123:881–4.
- Jacobs et al., Laboratory Test Handbook, Lexi‑Comp Inc, 1994.