Cerebrospinal Fluid (CSF) Cytology: Diagnostic Use in CNS Infections and Malignancies
What is Cerebrospinal Fluid (CSF) Cytology?
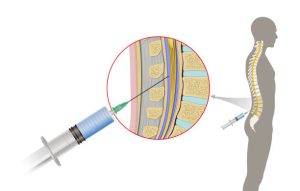
Cerebrospinal Fluid (CSF) Cytology (also called Spinal Fluid Cytology) involves microscopic evaluation of cells from cerebrospinal fluid obtained via lumbar, cisternal, or ventricular tap. It aids in diagnosing infections, neoplasms, and neurological disorders.
Synonyms:
Spinal Fluid Cytology
Applies To:
- Cisternal Tap Cytology
- Lumbar Tap Cytology
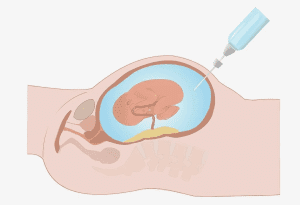
- Ventricular Tap Cytology
Test Commonly Includes:
Smears, filter preparations, cytocentrifuge preparations, and immunocytochemistry if clinically indicated.
Patient Care and Preparation:
- Obtain informed consent.
- Prepare the patient in a sterile field.
- Administer 1% lidocaine for local anesthesia.
Aftercare:
Monitor for complications like headache or vertigo. If persistent, a fibrin patch using the patient’s plasma may be required.
Specimen:
Fresh cerebrospinal fluid collected under sterile conditions.
Container:
Sterile screw-cap container or original collection tube from lumbar puncture tray.
Sampling Time:
30–60 minutes
Collection Procedure:
- Insert a 23-gauge spinal needle with stylet through the L1–L2 interspinous space.
- Collect fluid in 3 tubes. Send the third tube directly to cytology for analysis.
- Label all tubes with patient’s name, ID number, and date.
Storage and Handling:
Process immediately or fix 1:1 with Carbowax fixative if delay is expected. Cellular degeneration begins within 20 minutes at room temperature without fixation.
Causes for Sample Rejection:
- Improper or missing labeling
- Delayed transport (>3 hours at room temperature)
- Severe blood contamination
Special Instructions:
- Indicate sample origin and relevant clinical details (age, diagnosis, prior procedures).
- Inform the lab if the CSF is from a ventricular shunt.
Reference Range:
- Adults/Children: 0–5 mononuclear cells/μL
- Infants: 20–30 mononuclear cells/μL
Clinical Uses:
CSF cytology helps in the diagnosis of:
- Primary or metastatic CNS tumors
- Fungal infections (especially Cryptococcus)
- Bacterial, viral, and aseptic meningitis
- Demyelinating diseases like Multiple Sclerosis
- Leukemia:
- ~80% of untreated ALL patients may show leukemic cells
- ~60% of AML patients also show involvement
- Other malignancies: Lung, breast, kidney, GI, melanoma, choriocarcinoma
- HIV/AIDS-related CNS conditions: CMV, Cryptococcus, lymphoma (less so for Toxoplasma)
Limitations:
- Only tumors invading subarachnoid space or ventricles shed detectable cells.
- Metastatic tumors and leukemias are more easily detected than primary CNS tumors.
- Shedding is intermittent in meningeal lymphoma and carcinomatosis.
- Herpes meningitis cannot be diagnosed by cytology—requires brain biopsy.
Contraindications:
- Elevated intracranial pressure
- Abnormal coagulation profile
Additional Notes:
Myelography, radiation, and especially intrathecal chemotherapy can alter cytologic features significantly.
References:
- Bigner SH, Elmore PD, et al. Acta Cytol, 1985; 29(3):291.
- Bigner SH, Johnston WW. Cytopathology of the CNS, Masson Publishing, 1983.
- Wertlake PT, et al. Acta Cytol, 1972; 16:224–239.
- Jacobs, Demott, Finley, et al. Laboratory Test Handbook, Lexi-Comp Inc, 1994.