Urine Cytology: Diagnostic Approach to Urinary Tract Malignancies & Disorders
What is Urine Cytology?
Urine cytology is a non-invasive diagnostic test used to examine cells shed from the lining of the urinary tract. It helps detect cancers, infections, inflammatory conditions, and rare diseases of the urinary system.
Applies To:
- Voided Urine Cytology
- Catheterized Urine Cytology
- Bladder Washings Cytology
- Renal Pelvic Washings Cytology
- Ureteral Washings Cytology
- Pelvicocalyceal Barbotage Specimens
Test Usually Includes:
Smears, cytocentrifuge preparations, millipore filter preparations, flow cytometry, and immunocytochemistry.
Abstract:
Inflammatory, infectious, and cancerous conditions of the urinary tract can be evaluated using urine cytology.
Patient Care & Preparation:
- Hydrate the patient with several glasses of water 30–60 minutes prior to sample collection.
- Avoid use of mineral oil cathartics before testing.
- Discard the first morning urine due to prolonged bladder retention and aging of cells.
- Administer 1g of Vitamin C at bedtime the night before collection to improve cell preservation.
Specimen:
Freshly voided or catheterized urine, or urine obtained during surgical washing of the kidneys, ureters, or bladder.
Container:
Use a sterile, 100 mL plastic screw-top container. Transport immediately to the Cytology Laboratory.
Sampling Time:
Collect the freshest sample possible. Cellular degeneration starts within an hour at room temperature.
Collection Guidelines:
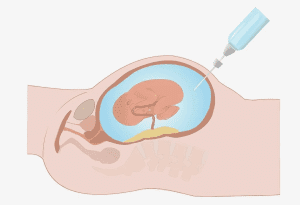
- For upper urinary tract lesions: catheterize each ureter to renal pelvis and collect samples individually.
- Use one ureter as a control during lesion localization.
- Label all samples as Right/Left ureter or pelvis.
- Send specimens to the Cytology Lab immediately.
Storage Instructions:
If immediate transport is not possible, refrigerate specimens at 4°C.
Causes for Sample Rejection:
- 24-hour urine collections
- Room temperature storage >1 hour
- Unlabeled or leaking container
- Visible contamination
Special Instructions:
- Catheterized samples preferred in females; voided urine preferred in males to avoid contamination.
- Avoid collecting bladder washings in hypotonic solution.
- Mention cytomegalovirus (CMV) suspicion on the requisition if clinically relevant.
Use:
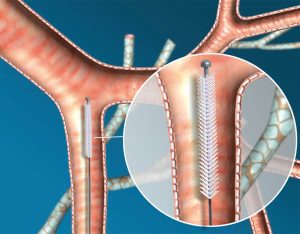
- Detect bladder tumors (especially high-grade transitional cell carcinoma)
- Identify malakoplakia, renal hemosiderosis, hemolytic anemia
- Diagnose cerebral metachromatic leukodystrophy and urinary tract endometriosis
- Evaluate recurrent urothelial carcinoma
- Assist in detecting metastatic cancers to the urinary tract
Limitations:
- Low-grade (Grade 1) transitional cell carcinomas may go undetected
- Recent instrumentation or presence of calculi can mimic malignancy
- Flow cytometry may fail to detect diploid tumors
- Drugs like BCG, Cytoxan, and thiotepa can produce dysplastic-like changes
- Low sensitivity for detecting prostate and primary renal tumors
- Complete clinical history is critical for accurate interpretation
Preferred Methods:
- Barbotage technique is most sensitive—uses gentle saline with air to exfoliate urothelium
- Combined cell morphology and DNA analysis improve diagnostic accuracy
- Flow cytometry may reveal aneuploidy or increased S-phase in transitional neoplasia
Additional Information:
Void urine is preferred over catheterized urine due to cell trauma from catheterization. Renal tubular cells may appear in acute tubular injury. Rarely, urine cytology helps diagnose lymphoma of the urinary tract.
References:
- Jacobs et al., Laboratory Test Handbook, Lexi-Comp Inc., 1994
- Betz SA et al., Am J Clin Pathol, 1993; 99(3):244-8
- Crosby JH et al., Acta Cytol, 1991; 35(3):263
- Eldidi MM & Patten SF, Acta Cytol, 1982; 26:725
- Koss LG et al., Hum Pathol, 1989; 20(6):528-48
- Murphy WM, Acta Cytol, 1982; 1(9):886