Cold Agglutinin Screen: Test Purpose, Collection, Use, and Interpretation
Specimen and Container
- Specimen: Blood
- Container: Red top tube
Causes of Sample Rejection
- Use of serum separator tube (SST)
- Gross hemolysis
- Incorrect or missing labeling on specimen tube
Reference Range
Negative: Titer less than 32
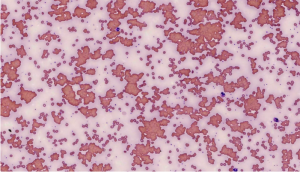
Use
This test is performed when a routine antibody screen or panel suggests the presence of cold autoagglutinins that may mask or interfere with identifying unexpected clinically significant antibodies. It is especially useful in suspected cold agglutinin disease, hemolytic anemia, or atypical pneumonia caused by infections such as Mycoplasma pneumoniae.
Methodology
- Serologic testing performed at both 4°C and room temperature
Additional Information
- Cold agglutinin titers assist in diagnosing certain infections and autoimmune hemolytic anemias.
- All individuals have naturally occurring cold hemagglutinins, but clinically significant ones react strongly at 4°C.
- Cold agglutinins that react at or above 20°C are considered to have a “wide thermal amplitude” and can cause:
- Hemolysis
- Thrombosis
- Agglutination
- Extremity pain
- They are often specific to the “I” antigen and may appear after certain infections.
- Cold autoagglutination can occur during cardiac surgery when perfusion temperatures range between 15°C and 32°C.
- This test is not used for transfusion compatibility but for diagnostic evaluation.
References
- Leach AB, Van Hasselt GL, Edwards JC. “Cold Agglutinins and Deep Hypothermia.” Anaesthesia. 1983;38:140–3.
- Diaz JH, Cooper ES, Ochsner JL. “Cold Hemagglutination Pathophysiology.” Arch Intern Med. 1984;144:1639–41.
- Heddle NM. “Acute Paroxysmal Cold Hemoglobinuria.” Transfus Med Rev. 1989;3(3):219–29.
- Roelcke D. “Cold Agglutination.” Transfus Med Rev. 1989;3(2):140–66.
- Jacobs, Demott, Finley, Horvat, Kasten JR, Tilzer. “Laboratory Test Handbook.” Lexi-Comp Inc, 1994.


