Gram Stain: Differential Staining for Bacterial Classification in Clinical Microbiology
Synonyms
Bacterial Smear, Smear for Gram Stain
Applies To
Crystal Violet, Safranin
Abstract
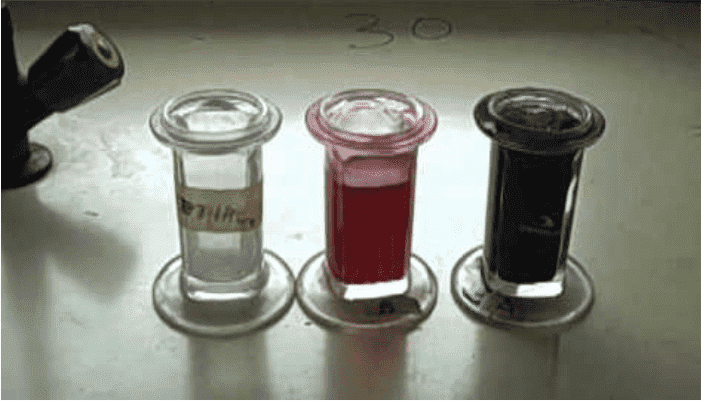
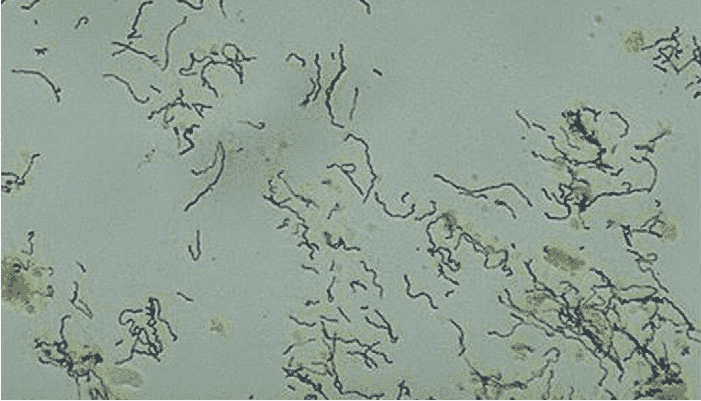
The Gram stain is a differential staining technique used to classify bacteria. Gram-positive bacteria retain the crystal violet dye and appear deep blue or purple. Gram-negative bacteria lose this stain and are counterstained with safranin, appearing red or pink. Accuracy depends on bacterial viability—aged or dead bacteria may stain atypically.
Patient Care / Preparation
Same preparation as the routine culture for the respective anatomical site.
Specimen
Duplicate of the sample collected for routine culture from the specific site.
Container
Sterile specimen container, sterile tube, or appropriate swab tube.
Collection
Collected aseptically, avoiding contamination from skin, adjacent structures, or unsterile surfaces.
Storage Instructions
Store the specimen as required for culture from the same site.
Reason to Reject Sample
Insufficient volume or improperly labeled specimen.
Turnaround Time
Usually the same day in most cases.
Special Instructions
Provide exact site, patient age, current antibiotic therapy, and clinical diagnosis to the lab.
Reference Range
Dependent on the specimen’s site; typically reported as organisms observed or not.
Use
- Rapidly detect and identify bacteria and yeast.
- Assess presence of neutrophils (infection) and epithelial cells (contamination).
- Critical in meningitis and pneumonia workups.
Limitations
- Does not replace culture for isolation and identification.
- Gram stain cannot detect Mycobacteria — requires acid-fast stain.
- Negative results in 20–30% of meningitis cases.
- Cannot reliably detect gonococcal infections in rectal, cervical, or pharyngeal samples.
Methodology: Gram Stain Technique
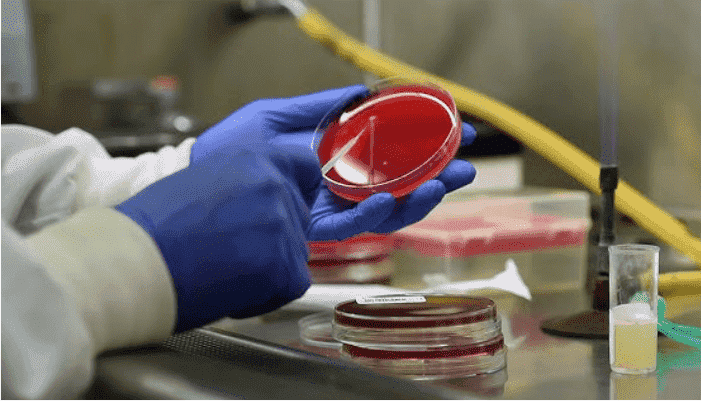
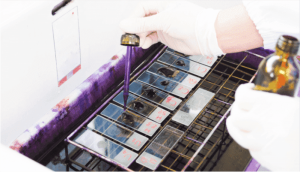
- Air-dry a thin smear of the specimen on a clean glass slide.
- Fix by passing through flame or using methanol/ethanol.
- Stain with crystal violet for 1 minute, then rinse.
- Add Gram’s iodine for 1 minute, then rinse again.
- Decolorize with acetone-alcohol until runoff is clear (approx. 10 seconds).
- Counterstain with safranin for 1 minute, then rinse.
- Air-dry and examine under 100x oil immersion objective.
- Gram-positive: Dark blue or purple
Gram-negative: Red or pink
Additional Notes
- Useful in early diagnosis of bacterial meningitis: 60–80% positivity in untreated cases.
- Squamous epithelial cells suggest contamination; >25/LPF in sputum sample deems it unsuitable for culture.
- Valid Gram stain requires quality sample — expectorated sputum with <25 epithelial cells/LPF and >25 PMNs/LPF.
- In CSF, Gram stain is the fastest, most reliable early test before culture or antigen detection.
- Mycobacteria are gram-neutral and need acid-fast staining.
- Low colony counts (~10,000/mL) in urine may appear as “few bacteria per HPF” in uncentrifuged samples.
References
- Koneman EW et al., Diagnostic Microbiology, 4th ed., JB Lippincott, 1992
- Gray LD, Fedorko DP, Clin Microbiol Rev, 1992
- Fishman RA, Cerebrospinal Fluid Disorders, WB Saunders, 1992
- Jacobs, Demott, Finley, Lab Test Handbook, Lexi-Comp Inc, 1994
- Durand ML et al., N Engl J Med, 1993; 328(1):21-8